 April 19, 2017 – For infertile couples, the expense, duration and low success rates of assisted reproduction can make the process a physical and emotional ordeal.
April 19, 2017 – For infertile couples, the expense, duration and low success rates of assisted reproduction can make the process a physical and emotional ordeal.
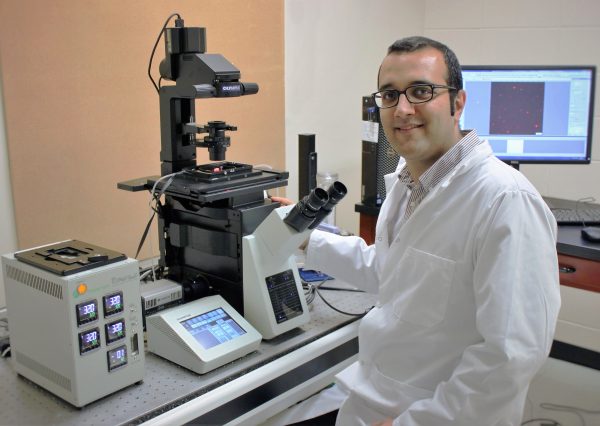
Reza Nosrati (MechE PhD 1T6), a postdoctoral researcher at Queen’s University aims to change that. Using microfluidics and advanced microscopy, he and his colleagues are developing simple but functional technologies for analysing and selecting sperm, and ultimately improving fertilization rates.
Much of his work has focused on male infertility. As a PhD candidate working under microfluidics expert Professor David Sinton at University of Toronto, one of his earliest projects was to design a simple, easy-to-use microfluidic device that would select sperm by “racing” the cells in microchannels. Winners of this race, when examined, showed 80% higher DNA integrity, making them potentially more successful in commercialized reproduction.
This research, which is now being commercialized, led to a subsequent project to characterize how sperm swim within a micrometre of surfaces. It was a significant challenge to capture their motion, he says, because sperm are very small and swim very fast.
In collaboration with a U of T expert in fluorescence microscopy, Professor Christopher Yip, he made an intriguing discovery: when moving close to the surface, human sperm adapt their swimming style from a 3D “corkscrew” motion to a more streamlined 2D “slither” movement that enables them to swim faster. This may be important to successful fertilization, says Nosrati. This was a major breakthrough in understanding sperm movement, and targeting slither swimmers has the potential to improve sperm selection for assisted reproduction.
His subsequent work focused on paper-based microfluidics to identify concentration of sperm, and their motility – how many of them move successfully from point A to B? The device works like a pH strip, used for testing acidity or alkalinity: reagent-coated sections on the paper strip react to a droplet of semen, changing color according to sperm concentration and motility. The latter is an important indicator of the sperm’s success at fertilization, and Dr. Nosrati’s test is the first to quantify that attribute.
Their long-term plan is to pair the device with a cell-phone application that could analyse and track semen quality day to day, enabling individuals to test themselves. “Family doctors could also use it as a first-step diagnostic,” he says. “There’s a lot of embarrassment and anxiety around this, and there aren’t any comprehensive products on the market.”
A related microfluidics device developed with Toronto colleague Dr. Max Gong, aims to diagnose overall sperm health, an important factor in fertilization success, using just a drop of semen. Current gold-standard clinical testing requires access to flow cytometry, an expensive technology that many fertility clinics do not have access to. “We came up with the idea of breaking up the sperm cells to get the DNA out, and then separating healthy and damaged DNA using an electric field.” This low-cost, paper-based approach showed 100% agreement with respect to clinical decision as compared with the flow cytometry-based assay.
While challenges remain – the device requires fluorescent microscopy and a power source – this approach shows potential as an affordable, self-administered alternative to current clinical testing.